 Chronic pain can feel like a life sentence — relentless, exhausting, and invisible. For many people, it takes multiple treatments to find out what works. Surgeries can fail. Physical therapy stalls. But now, there’s a fast-growing technology that is seeing increased adoption: Peripheral Nerve Stimulation (PNS).
Chronic pain can feel like a life sentence — relentless, exhausting, and invisible. For many people, it takes multiple treatments to find out what works. Surgeries can fail. Physical therapy stalls. But now, there’s a fast-growing technology that is seeing increased adoption: Peripheral Nerve Stimulation (PNS).
What was once a niche intervention for only the most complex cases is rapidly becoming a mainstream option for pain management. So, what exactly is PNS? Who can it help? And is it really as effective as some claim?
Let’s break it down.
What Is Peripheral Nerve Stimulation (PNS)?
How PNS Works
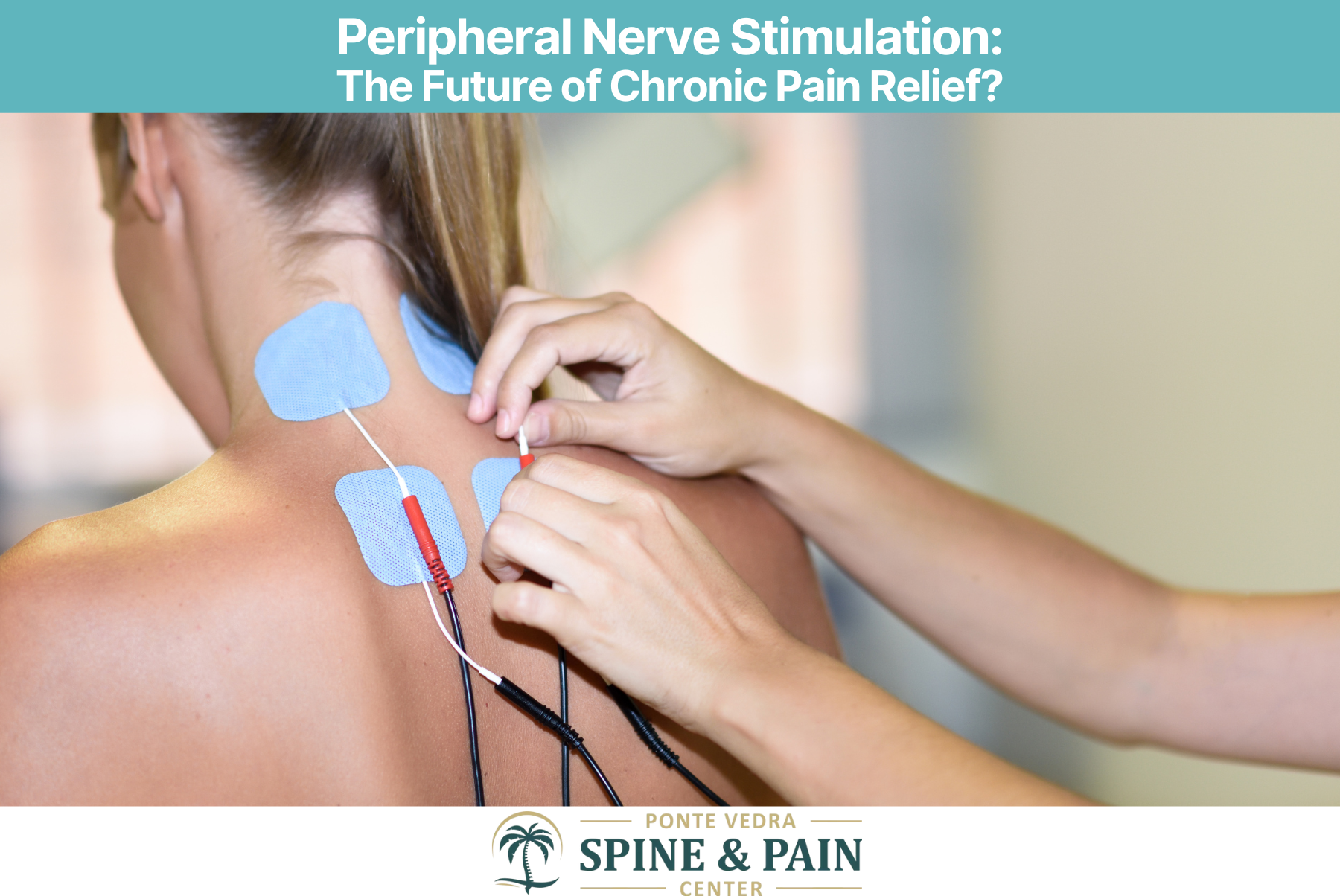
PNS involves placing a small electrical device that stimulates specific peripheral nerves — the nerves outside of your brain and spinal cord — using low-level electrical pulses.
These pulses disrupt the pain signals being sent to the brain with a goal of resetting the nerve. Think of it like a noise-cancelling headphone for your nervous system.
The Difference Between PNS and Spinal Cord Stimulation
Spinal Cord Stimulation (SCS) targets the spinal cord itself. PNS is more targeted — aimed at one or two specific nerves, which makes it ideal for focal pain (like pain in the knee, shoulder, or foot).
The Rise of PNS: Why It’s Gaining Popularity
The Chronic Pain Epidemic
Over 50 million Americans suffer from chronic pain. It’s the #1 reason people seek medical care — and it’s notoriously hard to treat.
Shift Toward Minimally Invasive Neuromodulation
PNS offers a non-destructive, drug-free option that’s both minimally invasive and reversible. That’s a game-changer in a world where patients are tired of failed surgeries and medication side effects.
Conditions That Can Be Treated with PNS
PNS isn’t just for one type of pain — it’s surprisingly versatile.
Post-Surgical and Post-Traumatic Pain
Patients who develop chronic pain after knee replacements, rotator cuff repairs, or nerve injuries often respond well to PNS.
Complex Regional Pain Syndrome (CRPS)
CRPS is one of the most severe and debilitating pain syndromes. PNS can be used to target the affected nerve, reducing both pain and hypersensitivity.
Migraine and Occipital Neuralgia
Targeting the occipital nerves at the base of the skull has shown promise in treating chronic migraines and cluster headaches.
Lower Back Pain and Sciatica
Yes, even certain types of back pain — especially when localized — can respond to targeted PNS of the lumbar or sacral nerves.
Peripheral Neuropathy and Amputee Pain (Phantom Limb)
PNS has been used to treat phantom limb pain and neuropathies where medications have failed.
Joint Pain
Chronic shoulder, knee, foot/ankle pain that is not amendable to surgery or has failed over treatment options can be treated with PNS.
Types of Peripheral Nerve Stimulation Devices
Temporary (Percutaneous) PNS
Some systems use temporary leads that are placed under the skin for 60 days, then removed. These options can still give pain relief for months or even years at a time. Great for initial treatments or for patients hesitant about a permanent implant.
Fully Implanted Systems
For long-term use, patients can get fully implanted pulse generators (IPGs) — similar to a pacemaker — with leads placed near the target nerve.
Wireless and Rechargeable Options
Modern systems are wireless, programmable, and in many cases, externally powered, eliminating the need for internal batteries or surgical battery replacements.
How the Procedure Works
The Trial Phase
Most PNS programs start with a trial period (usually 5–10 days). If it works well (often defined as >50% pain relief), the patient may move on to permanent implantation.
Permanent Implantation
The permanent device is implanted under local or mild sedation. Patients can go home the same day in most cases.
Pros of Peripheral Nerve Stimulation
Non-Destructive and Reversible
Unlike nerve ablation or surgeries, PNS doesn’t damage the nerve. If it doesn’t work or causes side effects, it can be turned off or removed.
Reduced Need for Opioids
PNS often allows patients to cut back or eliminate pain meds altogether — a huge win in the era of opioid caution.
Targeted Pain Relief
Because it stimulates only the affected nerve, PNS avoids systemic side effects that come with pills or whole-body stimulation.
Risks and Limitations
Lead Migration and Device Malfunction
Leads can shift over time, leading to reduced effectiveness or the need for reprogramming.
Incomplete Pain Coverage
PNS typically only helps localized pain. It’s not ideal for patients with widespread or diffuse pain.
Not a Cure, But a Tool
PNS doesn’t “fix” the underlying problem — it manages symptoms. It’s a tool, not a magic wand.
Research & Evidence: Does It Actually Work?
Clinical Trials and Meta-Analyses
A growing body of evidence supports the efficacy of PNS. A 2020 systematic review in Pain Medicine found consistent evidence that PNS provides significant pain relief in 50–70% of patients, especially for post-surgical and neuropathic pain.
How It Compares to Other Interventions
Compared to opioids and repeated nerve blocks, PNS has longer-lasting effects, fewer side effects, and lower long-term costs — especially when pain is localized.
Who Is a Good Candidate for PNS?
Ideal candidates include:
- Patients with chronic localized pain that hasn’t responded to meds or therapy
- Individuals not ready for surgery or who have failed surgery
- Patients seeking non-opioid options
- Those with good psychological readiness (anxiety/depression can reduce effectiveness)
The Future of PNS in Pain Medicine
We’re seeing a wave of innovation:
- AI-guided stimulation algorithms
- Smaller, more discreet devices
- Expanded indications (even bladder pain and pelvic pain are being explored)
As devices become smarter and more tailored, PNS could become first-line treatment for many pain syndromes.
Conclusion
Peripheral Nerve Stimulation isn’t just a flashy new gadget — it’s a meaningful, evidence-based advancement in pain medicine. It’s not for everyone, and it’s not a cure. But for the right patient, it can be life-changing.
If you’ve been living with chronic pain and feel like you’ve run out of options, it might be time to consider PNS.
FAQs
- Is peripheral nerve stimulation covered by insurance?
Yes, many insurers — including Medicare — cover PNS, especially if conservative treatments have failed. - Does PNS hurt?
Most patients report only mild discomfort during the procedure. The stimulation itself is typically a tingling or pulsing sensation, not pain. Some devices don’t produce any sensation at all. - Can PNS be removed later?
Yes, one of the biggest advantages of PNS is that it’s reversible. If it doesn’t work or causes side effects, it can be removed. - How long does PNS relief last?
For many, pain relief lasts as long as the device is functioning. Some experience prolonged benefit even after removal (due to neural desensitization). - Are there any side effects?
Most side effects are minor: skin irritation, lead migration, or battery issues. Serious complications are rare.
